Introduction
The brain is undoubtedly a complex organ that controls thought, memory, touch, motor skills, vision, breathing, temperature, and most other processes that regulate the body. As such, it needs a large amount of oxygen to function. The fact is that in a resting state about a fifth of the body’s total oxygen requirement is consumed through cerebral metabolism.
When the brain does not receive enough oxygen, brain cells can begin to die. Cell death can occur within 5 minutes of low oxygenation which quickly leads to various complications if oxygen is not redelivered. Since the brain is so complex and the process of hypoxia can occur so quickly, there is a great deal of preclinical research that goes into understanding these mechanisms and how to treat and mitigate damage due to cerebral hypoxia (or anoxia).
One way to investigate cerebral hypoxia caused by trauma (TBI) or lack of blood flow (stroke, MCAO) is to measure cerebral blood perfusion and pO2 directly within the area of interest. We at Oxford Optronix have been supporting brain research for 30+ years and helping researchers to answer these questions with our tissue vitality monitors to assess both parameters in real-time. Sensors start at a very fine 250 µm diameter making them minimally invasive.
This article looks at some of the major application areas in brain research and the large and small animal models used. We describe how our OxyLite and OxyFlo systems have been employed and we provide some supporting publications as reference material for the reader. Please note these systems can be used separately to garner microvascular blood flow or tissue pO2 information independently from separate tissue sites or in parallel using a unique combined sensor capable of reading pO2, blood flow and temperature from a singular site. There are also implantable sensors available for chronic studies and specialized sensors for use in an imaging setting like MRI and CT. These are discussed towards the end of this article.
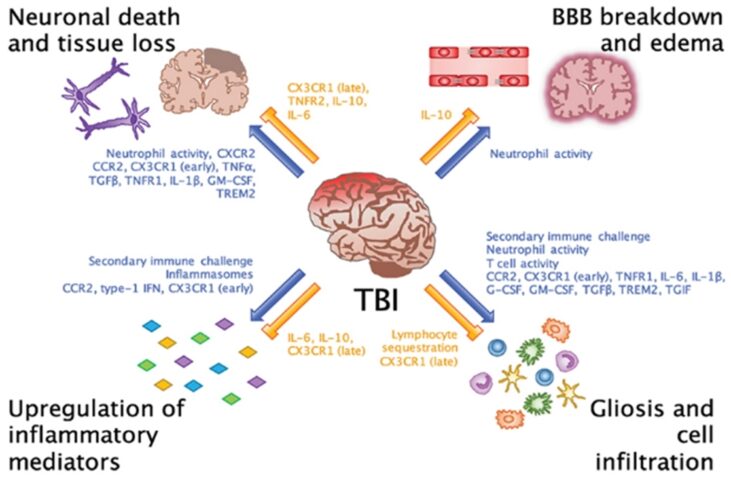
Traumatic brain injury (TBI) and tissue monitoring
Traumatic brain injury (TBI) is a sudden damage to the brain. It may happen when there is a blow, bump, or jolt to the head. Following head injuries there is reduction of cerebral blood flow (ischemia) which is detrimental to the brain’s ability to recover following the injury. Depending on the nature and severity of the injury, different approaches are often studied in animal models (of different sizes) to assess the feasibility and efficacy of a specific treatment.
The OxyLite™ and OxyFlo™ products have been used extensively over many years in these types of studies to assess brain health prior to, during, and following TBI. To further assess a treatment or the effect of a drug a researcher may look at the length of time it takes, following a traumatic event, for cerebral perfusion and brain pO2 return to a normal baseline.
Malik H, Wolff MD, Teskey GC, and Mychasiuk R (2022). Electrographic seizures and brain hyperoxia may be key etiological factors for postconcussive deficits. J of NeuroPhys. 128 (3), 727-737
Abutarboush R, Mullah SH, Saha BK, Haque A,Peter B, … McCarron RN, Scultetus AH, Moon-Massat P (2018). Brain oxygenation with a non-vasoactive perfluorocarbon emulsion in a rat model of traumatic brain injury. Microcirculation 25 (3), e12441
Schilte C, Bouzat P, Millet A, Boucheix P, Pernet-Gallay K, Lemasson B, Barbier EL and Payen JF (2015). Mannitol Improves Brain Tissue Oxygenation in a Model of Diffuse Traumatic Brain Injury. Crit Care Med 43(10), 2212-8
Teranishi K, Scultetus A, Haque A, Stern S, Philbin N, Rice J, Johnson T, Auker C, McCarron R, Freilich D and Arnaud F (2012). Traumatic brain injury and severe uncontrolled haemorrhage with short delay pre-hospital resuscitation in a swine model. Injury 43(5), 585-93
Stroke/MCAO and tissue monitoring
A stroke, also known as a transient ischemic attack, happens when blood flow to the brain is blocked. This prevents a region of the brain receiving oxygen and nutrients from the blood. Without oxygen, brain cells begin to die within minutes.
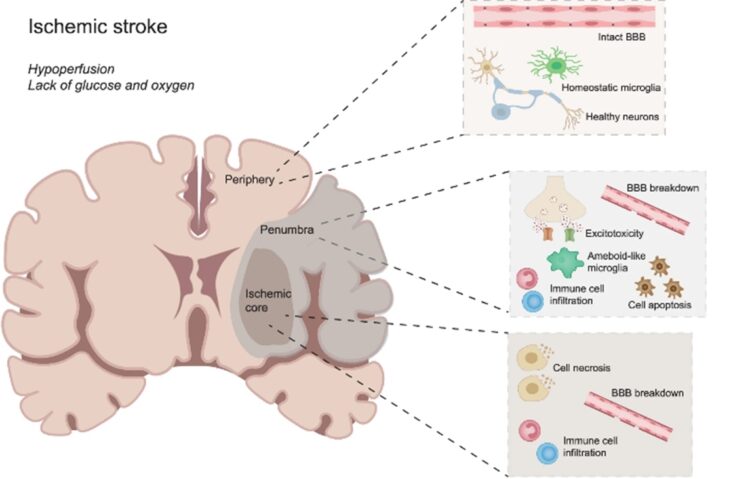
As a stroke can cause lasting brain damage, long-term disability, or even death, it’s important to quickly mitigate the damage. This can be achieved by reperfusion (unblocking the stroke site) or using methods that extend brain cell survival, which is a focus for a large portion of translational research. Very much like in trauma studies where TBI researchers use the OxyLite™ and OxyFlo™ to assess brain health, in stroke models the same instruments and sensors can also be employed to assess (and quantify) the extent of the ischemic insult and to observe a potential or complete recovery to baseline following a drug or treatment intervention.
Nizari S, Basalay M, Chapman P, Korte N, Korsak A, Christie IN, Theparambil SM, Davidson SM, Reimann F, Trapp S, Yellon DM , Gourine AV (2021). Glucagon-like peptide-1 (GLP-1) receptor activation dilates cerebral arterioles, increases cerebral blood flow, and mediates remote (pre)conditioning neuroprotection against ischaemic stroke. Basic Res Cardiol 116 (32)
Poon YY, Liu YW, Huang YH, Chan SH, Tsai CY (2021). Postoperative Stroke after Spinal Anesthesia and Responses of Carotid or Cerebral Blood Flow and Baroreflex Functionality to Spinal Bupivacaine in Rats. Biology 10 (7), 617
Chen CC, Chang CP, Yang CL (2019) An adaptive fall-free rehabilitation mechanism for ischemic stroke rat patients. Scientific Reports 9, 984
Suh JY, Cho G, Song Y, Woo DC, Choi YS, Ryu EK, Park BW, Shim WH, Kim YR, Kim JK (2018). Magnetic Resonance Imaging Biomarker to Assess Cerebral Oxygenation and Ischemic Damage in Stroke. Stroke 49, 3012–3019
Brain damage caused by other diseases or ailments assessed by tissue monitoring
Cerebral vitality assessment using the OxyLite™ and OxyFlo™ devices can also provide valuable surrogate data during trauma elsewhere in the organism or to other vital organs, e.g., during episodes of sceptic shock and/or resuscitation. Since the brain is such an important organ overall, monitoring it even peripherally can provide researchers with useful information on general health or on the efficacy of a specific treatment.
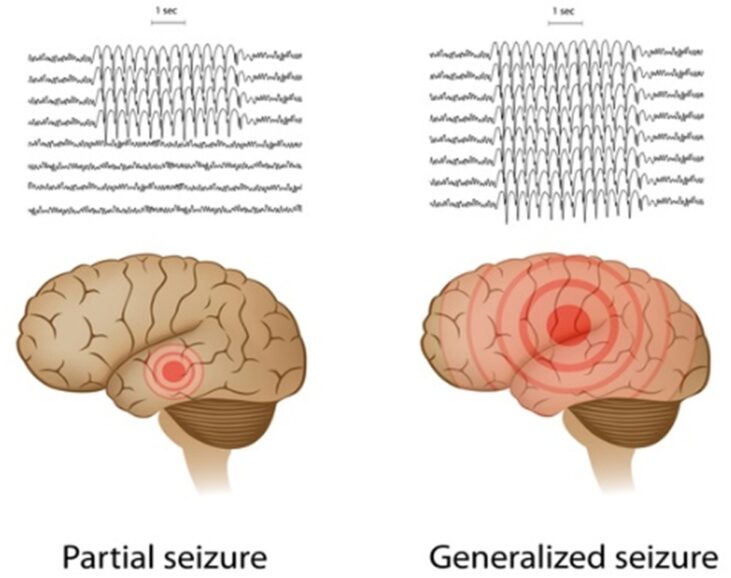
Other ailments, like haemorrhage, seizures, and epilepsy that originate in the brain can often cause a change in intracranial pressure, cerebral perfusion, and oxygenation. Being able to monitor these vital physiological parameters is potentially of great value to the clinical scientist in models of drug treatment or other intervention.
Seizure
Malik H, Wolff MD, Teskey GC, and Mychasiuk R (2022) Electrographic seizures and brain hyperoxia may be key etiological factors for post-concussive deficits. J of NeuroPhys. 128 (3), 727-737
Jansen NA, Schenke M, Voskuyl RA, Thijs RD, van den Maagdenberg J, Tolner EA (2019). Apnea associated with brainstem seizures in Cacna1as218l mice is caused by medullary spreading depolarization. J of Neuroscience 39 (48), 9633-9644
Hemorrhage
Yang LY, Chen YR, Lee JE, Chen KW, Luh HT, Chen YT, Wang KC, Hsieh ST (2022). Dental Pulp Stem Cell-Derived Conditioned Medium Alleviates Subarachnoid Hemorrhage-Induced Microcirculation Impairment by Promoting M2 Microglia Polarization and Reducing Astrocyte Swelling. Transl Stroke Res.
Other
Wang CH, Huang CH, Tsai MS, Wang CC, Chang WT, Liu SH, Chen WJ (2022). Inhaled Carbon Dioxide Improves Neurological
Outcomes by Downregulating Hippocampal Autophagy and Apoptosis in an Asphyxia-Induced Cardiac Arrest and Resuscitation Rat Model. J Am Heart Assoc. 11(21):e027685
Boorman LW, Samuel, Harris SS, Shabir O, Lee L, Eyre B, Howarth C, Berwick J (2022). Bidirectional alterations in brain temperature profoundly modulate spatiotemporal neurovascular responses in-vivo: Implications for theragnostics. bioRxiv
Other applications in brain research
Implantable sensors for tissue monitoring
For those performing chronic studies of the brain, implantable sensors offer a way to take serial measurements over time. In short, the sensors need to be surgically implanted into the brain. After a period of recovery measurements can be taken in awake, restrained, or anesthetized models by connecting the miniature exteriorized sensor ferrule to a dedicated adapter, itself attached to the OxyLite™ oxygen monitor.

Yu LH, Thurston EMS, Hashem M, Dunn JF, Whelan PJ and Murari K (2020). Fiber photometry for monitoring cerebral oxygen saturation in freely-moving rodents. Biomedical Optics Express 11 (7), 3491-3506
Malik H, Wolff MD, Teskey GC, and Mychasiuk R (2022) Electrographic seizures and brain hyperoxia may be key etiological factors for postconcussive deficits. J of NeuroPhys. 128 (3), 727-737
Lee K, Bohnert S, Vair C, Mikler J, and Dunn JF (2020). Cerebral blood flow and oxygenation in rat brain after soman exposure. Toxicol Lett 336, 50-56. doi: 10.1016/j.toxlet.2020.10.009
MRI compatible sensors
Advanced imaging techniques, like magnetic resonance imaging, continue to be commonly used to examine the anatomy and physiological processes of the brain. Researchers using these imaging techniques commonly wish to validate their data. As the OxyLite™ and OxyFlo™ sensors utilize fibre optic technology, they are fundamentally MRI compatible, allowing for real-time blood flow and tissue oxygen measurement even during MRI. Dedicated, extended length sensors are available for this application.
